This post has been read 1044 times!
 December 23, 2021- by Steven E. Greer, MD
December 23, 2021- by Steven E. Greer, MD
My father recently left the hospital after almost two-weeks with COVID. His main problem in and out of the hospital was severe dementia brought on by the virus. He then suddenly got back to his old baseline and improved. It was like a light switch was flipped on.
His dementia was not just the type brought on by the hospital setting (i.e., lack of outdoor visual queues, lack of long REM sleep, etc.) because a fancy hospital room with a window did not help, and he did not get better at home for many days. It made me wonder about the virus and effects on brain cells.
Here are some new papers on it:
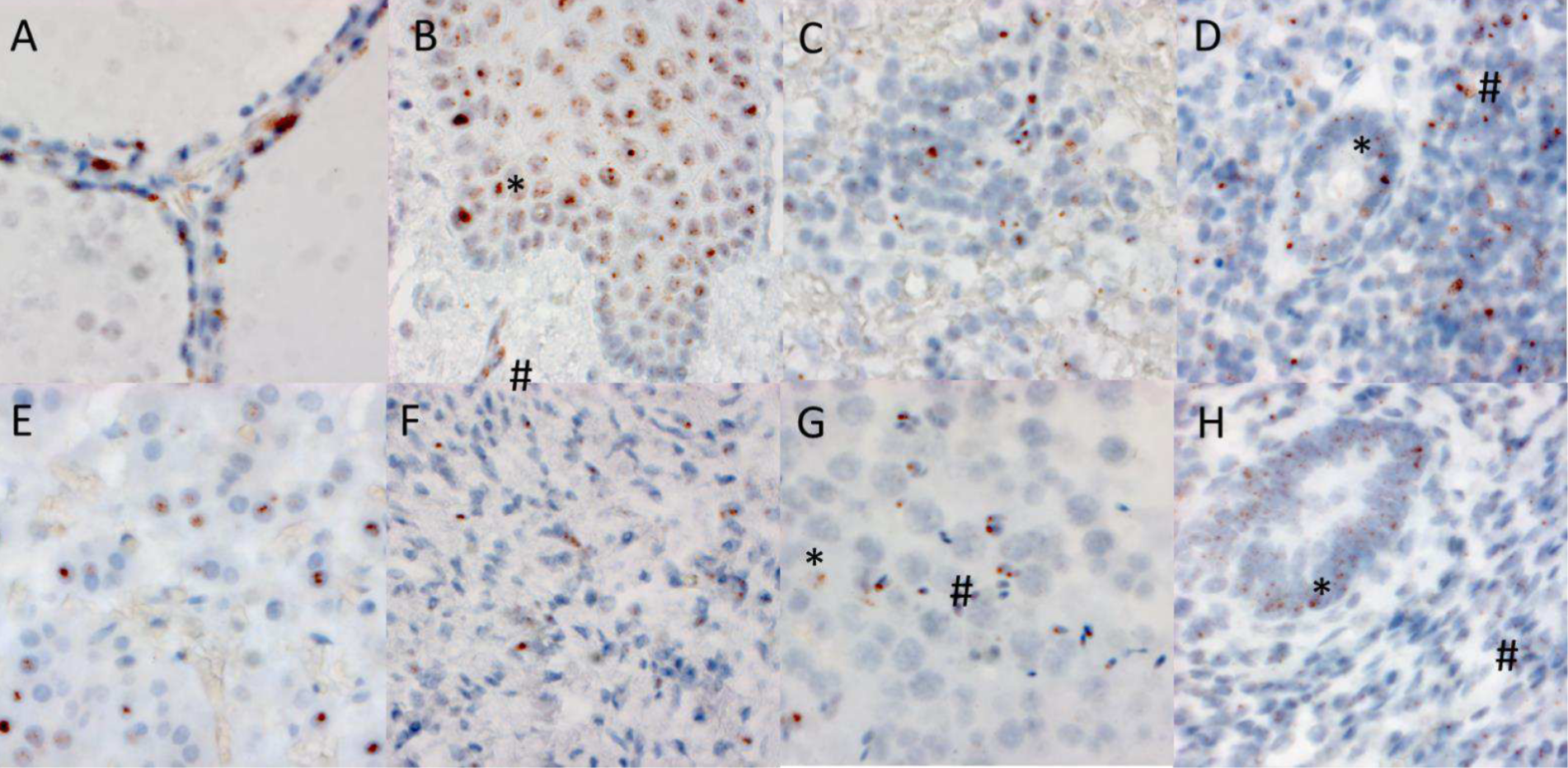
Neuroinvasion of SARS-CoV-2 in human and mouse brain
SARS-CoV-2 infection and persistence throughout the human body and brain, 2021, Chertow et al
The second one shows that the virus still replicates for 6-months after recovery.
Maybe we should treat with oral therapies after the patient has recovered from the acute phase to stop this viral replication that persists.
In reality, almost no COVID patient is currently receiving any oral therapy, whether it be the new Pfizer or Merck pills, ivermectin, etc. Would early treatment with oral therapies prevent the 6-month replication described in the second paper above? Would a short course of oral therapy work or would it need to be longer? This needs to be studied.
Now that profitable drugs have been approved (as opposed to generic ivermectin, hydroxychloroquine, etc. ), one can be sure that Pfizer will be studying this. Look for vaccines to be forgotten by the Pfizer marketing machine and oral therapies to be the new drug pushed.
Update September 15, 2022- The journal Nature confirms the hydroxychloroquine works to prevent SARS-CoV-2 from entering cells