This post has been read 2015 times!
- OPINION Wall Street Journal
- Updated June 4, 2012, 7:19 p.m. ET
Inside ObamaCare’s Grant-Making
Early this year, I was briefly involved with one of the Affordable Care Act’s bureaucracies called the Center for Medicare and Medicaid Innovation, or CMMI. Despite its lofty ideals, it is one more pork program and venue for political cronyism, as I learned firsthand.
The innovation center is supposed to test better ways to deliver and pay for health care than the current fee-for-service system, and the outfit will spend $10 billion over the next decade on awards, grants and contracts. In a recent letter to Congress defending its work, the center touted its “structured clearing process” and “rigorous evaluation of models.” But I found there are few safeguards and little transparency in practice.
This January, I was invited to review grant applications for something called the Health Care Innovation Challenge. Local health systems, state Medicaid programs and the like could apply for awards ranging from $1 million to $30 million, with priority for “projects that rapidly hire, train and deploy new types of health care workers.” I was selected to become one of the chairmen overseeing the volunteer panels of outside experts. Our grant application reviews were supposed to help the CMMI in making the final award decisions. There were more than 3,000 grant applications in total.
Having written numerous other federal grant applications as a medical researcher, I was surprised by the very short time allotted to review 12 applications, each of which ran more than 100 pages. We had only two weeks to assemble a team and grade the applications on such criteria as the promise of the project design and its workforce goals.
Applications to the government’s National Institutes of Health or the Patient-Centered Outcomes Research Institute, by contrast, undergo months of thoughtful review by scientists who are well-regarded in their fields. I began to wonder how much CMMI was interested in high-quality input from the grant reviewers.
To make matters more challenging, the computer system that handled our grant-scoring input was malfunctioning and deleting the painstaking comments and scores that our reviewers were inputting. When I reported the problems to the outside IT contractor, a support technician accused me and my team of never writing the reviews in the first place. All but one of my reviewers quit due to the digital hassle and the time-consuming workload.
That is when I sent a memo to CMMI Director Richard Gilfillan and Health and Human Services Secretary Kathleen Sebelius. I said that the rushed process was simply collecting “junk in, junk out” reviews. When I received no response, I left the CMMI program as well. Based on my experience, it seems unlikely that the 3,000 applications were closely vetted.
In May, the innovation center announced the first batch of grant recipients, 26 in all. George Washington University earned $1,939,127 because it expected to reduce health costs by a mere $1.7 million. Similarly, the Center for Health Care Services in San Antonio received $4,557,969 to save $5 million. At least CMMI didn’t pick one of the thinly veiled handout requests that I personally oversaw, such as a for-profit company that claimed to offer holistic healing through human touch.
Of particular note was a $5,862,027 grant to the University of Chicago medical center to “train and create new jobs for an estimated 90 individuals from this high-poverty, diverse community.” The program is part of the school’s Urban Health Initiative. Perhaps creating this is a noble use of federal funds, but job creation seems far afield from the CMMI mission to innovate.
Dr. Donald Berwick was Administrator of the Centers for Medicare and Medicaid Services from July 2010 to December 2011. CMMI, which was established during his tenure, started another program called the Partnership for Patients. That $500 million initiative is supposed to reduce hospital-acquired conditions and hospital readmissions.
In December 2011, the Partnership for Patients awarded a contract to the Health Research and Education Trust, which in turn awarded a subcontract to the Boston-based Institute for Healthcare Improvement—which Dr. Berwick ran for 19 years before he moved to Medicare. A source involved with Partnership for Patients told me about the relationship.
I emailed Dr. Berwick in May to confirm the subcontracts between the institute and the trust. “I don’t think there are contracts between them, but they’re good friends,” he replied. He was careful to note that he is no longer the institute’s CEO, though he now works out of the institute’s Boston offices as an adviser. The Health Research and Education Trust and the Institute for Healthcare Improvement have not responded to requests for information about the subcontract.
Even if the innovation center’s grants were chosen via a squeaky-clean peer-review system and awarded solely on merit, they would still be a waste of taxpayer money because Medicare should not be straying from its core competencies into areas like job creation. Congress ought to dismantle and defund the program if CMMI survives the Supreme Court ruling on the Affordable Care Act.
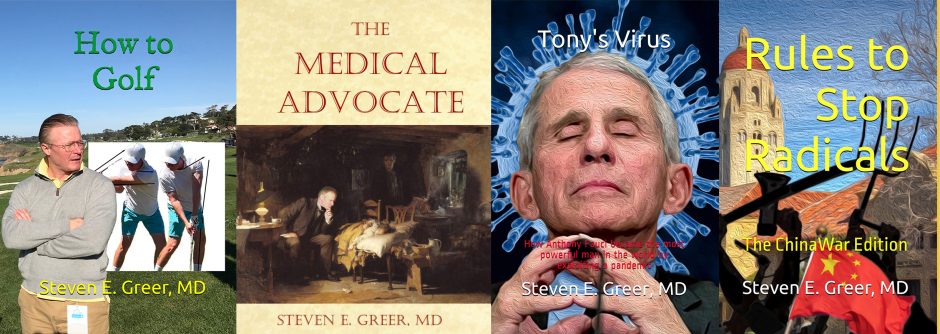
Dr. Greer, a surgeon, is CEO of the Healthcare Channel (thehcc.tv) and a financial analyst.